Fundamentals of Nursing provides a comprehensive introduction to the profession, covering essential concepts, skills, and practices. It serves as a foundation for understanding patient care, nursing theories, and evidence-based practice.
Overview of Nursing as a Profession
Nursing is a dynamic profession that combines science and art to provide holistic care to individuals, families, and communities. It involves promoting health, preventing illness, and managing various health conditions.
Nurses play a critical role in healthcare systems, working collaboratively with interdisciplinary teams. The profession requires strong communication skills, empathy, and critical thinking to address diverse patient needs effectively.
Key Concepts and Theories in Nursing Practice
Nursing practice is grounded in essential concepts such as safety, comfort, and patient-centered care. Theories like Florence Nightingale’s environmental theory and Jean Watson’s caring theory guide evidence-based practice. These frameworks emphasize holistic care, addressing physical, emotional, and spiritual needs. Nurses use these theories to assess, plan, and implement care tailored to individual patient needs, ensuring effective and compassionate outcomes.

The Nursing Process
The nursing process is a patient-centered, systematic method of delivering care. It involves assessment, diagnosis, planning, implementation, and evaluation to achieve optimal patient outcomes.
Assessment, Diagnosis, Planning, Implementation, and Evaluation
The nursing process begins with assessment, gathering patient data to identify health needs. Diagnosis involves formulating care priorities based on assessment findings. Planning sets realistic goals and interventions. Implementation executes the care plan, while evaluation assesses its effectiveness and patient outcomes. This structured approach ensures individualized, evidence-based care, promoting continuity and improving patient well-being. Each phase is interconnected, ensuring comprehensive and patient-centered care delivery.
Patient-Centered Care and Critical Thinking
Patient-centered care focuses on tailoring interventions to meet individual needs, ensuring dignity, and promoting autonomy. Critical thinking involves analyzing patient data, prioritizing concerns, and making sound decisions. Nurses integrate evidence-based practices with ethical considerations to deliver holistic care. This approach fosters collaboration between patients and healthcare providers, enhancing care quality and patient satisfaction. By combining empathy with analytical skills, nurses provide compassionate, effective, and personalized care, addressing physical, emotional, and social dimensions of health.

Contemporary Healthcare Environment
The contemporary healthcare environment integrates technology, evidence-based practices, and diverse care settings to address complex patient needs and evolving policies effectively.
Healthcare Settings and Delivery Systems
Healthcare settings vary widely, including hospitals, clinics, long-term care facilities, and community health organizations. Each setting requires tailored nursing approaches to meet patient needs. Delivery systems emphasize coordination and accessibility, ensuring seamless care transitions. Nurses must adapt to diverse environments, from acute care to rehabilitation, while maintaining high standards of patient-centered care. The integration of technology and interdisciplinary collaboration further enhances the efficiency of these systems, ensuring comprehensive and effective healthcare delivery.

Technological Advancements in Nursing Practice
Technological advancements are transforming nursing practice, enhancing patient care and operational efficiency. Electronic Health Records (EHRs) streamline documentation, improving data accuracy and accessibility. Wearable devices and telehealth platforms enable remote monitoring, expanding care reach. Automated medication systems reduce errors, while robotic assistants aid in tasks like lifting. These innovations not only improve patient outcomes but also support nurses in delivering high-quality, evidence-based care, fostering a safer and more effective healthcare environment.
Legal and Ethical Issues in Nursing
Nursing involves navigating legal and ethical challenges, including patient rights, confidentiality, and informed consent. Understanding these principles ensures safe, respectful, and accountable patient care practices.
Professional Responsibilities and Accountabilities
Nurses are accountable for delivering high-quality care, adhering to ethical standards, and upholding professional competencies. They must maintain patient safety, respect confidentiality, and take responsibility for their actions. Accountability involves accurate documentation, continuous learning, and collaboration with healthcare teams. Professional responsibilities include promoting health, preventing illness, and advocating for patients’ rights. Nurses must also comply with legal regulations and organizational policies, ensuring transparency and integrity in their practice. These responsibilities are fundamental to building trust and ensuring optimal patient outcomes.
Privacy, Confidentiality, and Informed Consent
Respecting patient privacy and confidentiality is a cornerstone of nursing ethics. Nurses must safeguard personal health information and only disclose it with proper authorization. Informed consent ensures patients are fully aware of their care options, risks, and benefits, enabling them to make autonomous decisions. Nurses play a key role in educating patients and obtaining consent, while adhering to legal and ethical guidelines. Maintaining trust through these practices is essential for providing person-centered care and upholding professional standards.
Patient Care and Safety
Patient care and safety are prioritized through evidence-based practices, ensuring safe environments and preventing harm. Nurses implement measures to promote well-being and recovery effectively.
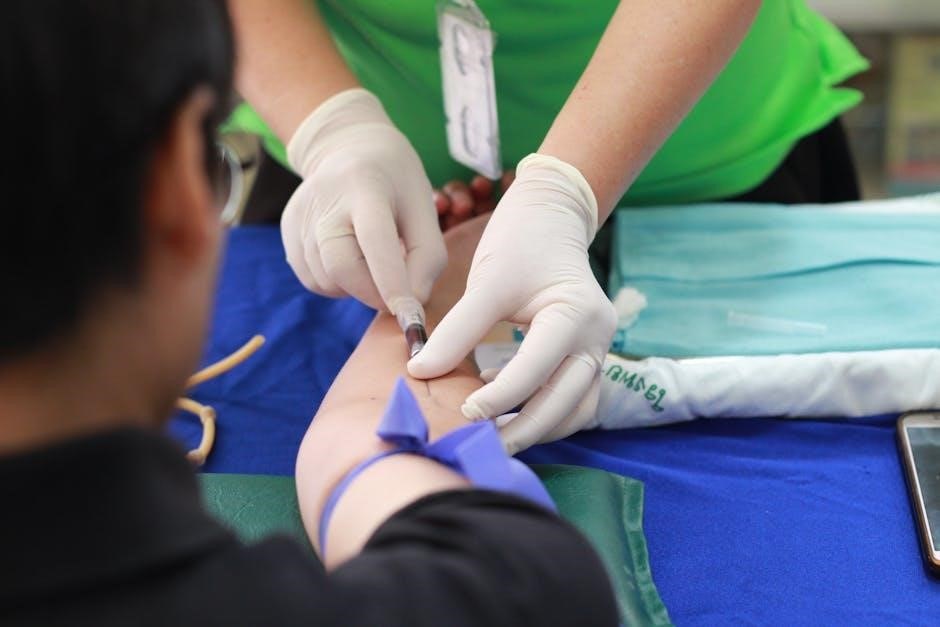
Safety Measures and Risk Management
Safety measures in nursing are crucial to prevent harm and ensure a secure environment for patients. Risk management involves identifying potential hazards and implementing strategies to mitigate them. Nurses use tools like safety protocols, checklists, and continuous monitoring to minimize risks. Effective communication and teamwork are essential to address adverse events promptly. Ongoing education and training help nurses stay updated on best practices, ensuring high standards of patient safety and care. These measures collectively enhance patient outcomes and reduce complications, fostering a culture of safety in healthcare settings.
Pain Management and Comfort
Pain management is a critical aspect of nursing care, focusing on assessing and alleviating discomfort to improve patient well-being. Nurses use pharmacological and non-pharmacological interventions, such as analgesics, relaxation techniques, and positioning strategies. Individualized care plans are developed to address the unique needs of each patient, ensuring effective pain relief and enhanced comfort. Regular reassessment and documentation of pain levels help in adjusting interventions, promoting optimal outcomes and improving quality of life for patients experiencing acute or chronic pain.

Nutrition and Hydration in Nursing Care
Nutrition and hydration are essential for patient recovery and overall health. Nurses assess needs, develop care plans, and provide interventions to ensure proper dietary intake.
Importance of Nutrition in Patient Recovery
Nutrition plays a vital role in patient recovery, aiding tissue repair and immune function. Adequate food intake helps prevent malnutrition, reducing complications and hospital stays. Nurses assess dietary needs, monitor intake, and provide tailored plans to optimize recovery. Proper nutrition enhances strength, wound healing, and overall well-being, ensuring patients regain health effectively. Malnutrition can delay recovery, making it crucial for nurses to address dietary needs proactively, promoting faster healing and better patient outcomes.
Fluid and Electrolyte Balance
Fluid and electrolyte balance is crucial for maintaining homeostasis, regulating bodily functions, and preventing complications. Nurses monitor hydration levels, assess for imbalances, and provide tailored interventions. Electrolytes like sodium, potassium, and calcium are essential for nerve function and muscle contractions. Imbalances can lead to serious conditions, such as arrhythmias or seizures. Nurses play a key role in managing IV fluids and educating patients on hydration, ensuring optimal recovery and overall health. Proper balance supports cellular health and bodily systems, preventing adverse outcomes.

Elimination and Continence Care
Elimination and continence care focuses on managing urinary and bowel processes, ensuring proper function and dignity. Nurses assess and address incontinence, promoting comfort and hygiene through tailored interventions and education.
Urinary and Bowel Elimination
Urinary and bowel elimination are essential bodily functions requiring careful nursing assessment and care. Nurses monitor normal elimination patterns, addressing factors like fluid intake, diet, and mobility that may influence them. Abnormalities, such as constipation or urinary retention, are identified and managed through interventions like dietary adjustments, hydration, or medication. The nursing process ensures individualized care, promoting comfort and preventing complications. Patient education on healthy habits and bowel training is also a key component of holistic nursing practice in this area.
Management of Incontinence
Management of incontinence involves a comprehensive approach to address urinary or bowel incontinence, focusing on assessment, individualized care plans, and non-pharmacological interventions. Nurses assess the type, severity, and underlying causes of incontinence, developing strategies to restore or manage elimination patterns. Interventions include pelvic floor exercises, timed voiding, and the use of assistive devices like catheters or incontinence products. Patient education on lifestyle modifications, such as fluid management and diet adjustments, is crucial. Pharmacological treatments may also be integrated to enhance bladder or bowel control, ensuring dignity and comfort for patients.
Education and Career Development in Nursing
Education is vital for nursing, promoting professional growth and expertise; Continuous learning through textbooks, online resources, and courses ensures adaptability in dynamic healthcare environments.
Role of Education in Nursing Practice
Education is the cornerstone of nursing practice, providing foundational knowledge and skills. It equips nurses with evidence-based practices, critical thinking, and patient care expertise. Nursing textbooks, online resources, and courses offer comprehensive learning tools. Education fosters effective communication, ethical decision-making, and adaptability. It ensures nurses stay updated on healthcare advancements, enhancing their ability to deliver high-quality, safe care. Continuous learning through structured programs and real-world applications prepares nurses to meet evolving patient needs and professional challenges effectively.
Continuous Professional Development
Continuous professional development is vital for nurses to stay updated with healthcare advancements. It involves ongoing education, training, and skill enhancement. Nurses engage in workshops, conferences, and online courses to expand their knowledge. Structured programs and evidence-based research foster improved patient outcomes. Professional development also includes reflective practice, peer learning, and adapting to new technologies. It ensures nurses remain competent, deliver high-quality care, and meet evolving patient needs. Lifelong learning is essential for maintaining professional standards and addressing complex healthcare challenges effectively.

